Explanation of varicose veins.
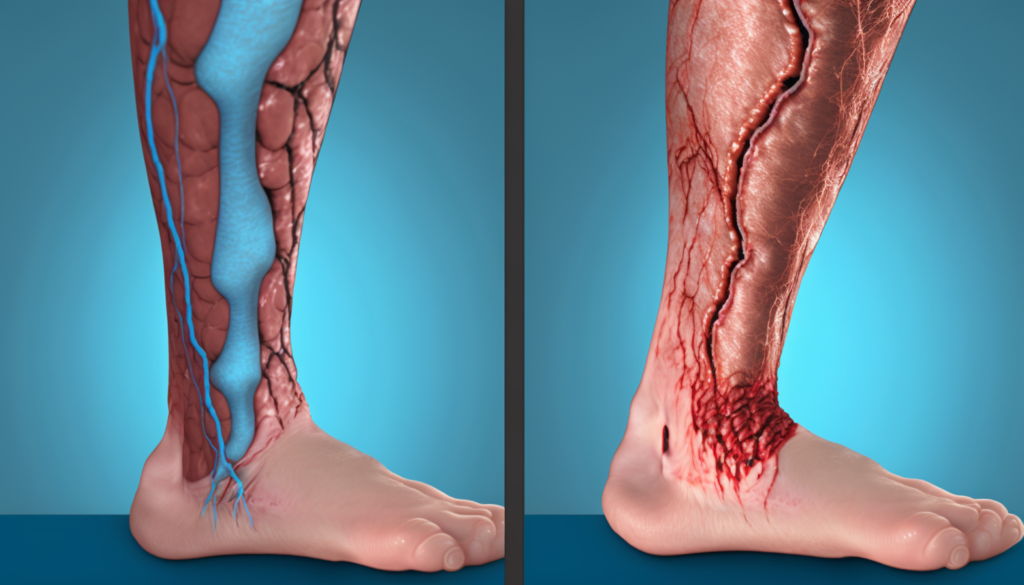
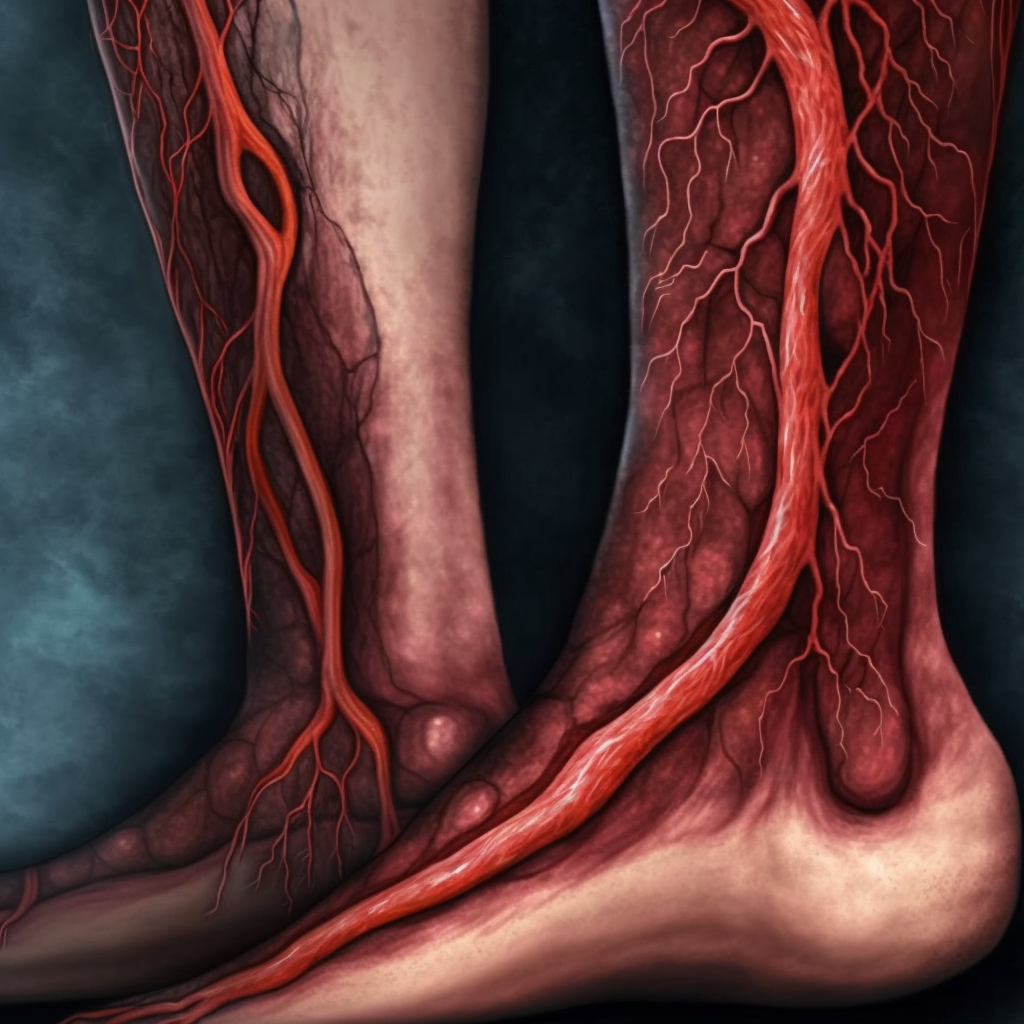
Varicose veins are enlarged, twisted, and swollen veins that appear blue or purple in color. They usually occur in the legs and feet, but can also develop in other parts of the body. Varicose veins are a common condition that affects up to 30% of adults. They can cause discomfort, pain, and swelling, and can also be a cosmetic concern for some people. Varicose veins occur when the valves in the veins that help regulate blood flow become weak or damaged, causing blood to pool in the veins and leading to their enlargement and twisting. Factors such as genetics, age, gender, obesity, pregnancy, and occupations that involve prolonged sitting or standing can increase the risk of developing varicose veins.
Importance of managing and preventing varicose veins.
Managing and preventing varicose veins is important for several reasons. First, varicose veins can cause discomfort, pain, and swelling, which can negatively affect a person’s quality of life. Second, they can increase the risk of developing other conditions, such as blood clots, skin ulcers, and deep vein thrombosis (DVT). Third, varicose veins can be a cosmetic concern, leading to feelings of self-consciousness and decreased self-esteem. Finally, untreated varicose veins can lead to more serious health problems, such as chronic venous insufficiency, which can result in long-term damage to the veins and surrounding tissues. Therefore, it is important to manage and prevent varicose veins through lifestyle changes, such as exercise and weight management, and seek medical treatment if symptoms persist or worsen.
Genetics.
Genetics can play a role in the development of varicose veins. If a person has a family history of varicose veins, they are more likely to develop the condition themselves. This is because the tendency to develop weakened valves in the veins can be passed down from generation to generation. Additionally, certain genetic factors can affect the strength and elasticity of the veins, making them more prone to damage and inflammation. While genetics is just one of the many risk factors for varicose veins, it is important for people with a family history of the condition to be aware of their increased risk and take steps to manage and prevent it.
Age.
Age is a risk factor for varicose veins. As people age, the veins in their legs can lose their elasticity and become weaker, making them more susceptible to damage and inflammation. Additionally, the valves in the veins can become less effective over time, leading to blood pooling in the veins and causing them to enlarge and twist. Varicose veins are more common in older adults, with the highest incidence occurring in people over the age of 50. While aging is a natural process that cannot be avoided, there are steps that people can take to manage and prevent varicose veins, such as regular exercise and weight management.
Gender.
Gender is another risk factor for varicose veins. Women are more likely to develop varicose veins than men, with an estimated 55% of women experiencing the condition at some point in their lives. This is partly due to hormonal factors, as female hormones such as estrogen and progesterone can weaken the walls of the veins and make the valves less effective. Pregnancy is also a risk factor for varicose veins in women, as the increased pressure on the veins in the pelvis and legs can cause them to enlarge and twist. While gender is a risk factor that cannot be changed, women can take steps to manage and prevent varicose veins, such as wearing compression stockings and staying physically active.
Obesity.
Obesity is a risk factor for varicose veins. When a person is overweight or obese, there is increased pressure on the veins in the legs, which can cause them to weaken and become damaged. This can lead to the development of varicose veins. Additionally, excess body weight can increase the risk of developing other conditions that can contribute to varicose veins, such as high blood pressure and diabetes. Maintaining a healthy weight through a balanced diet and regular exercise can help to manage and prevent varicose veins. Losing weight can reduce the pressure on the veins in the legs and improve overall circulation, which can reduce the risk of developing varicose veins.
Pregnancy.
Pregnancy is a risk factor for varicose veins. During pregnancy, the body produces more blood to support the growing fetus, which can increase the pressure on the veins in the legs and pelvis. This increased pressure can cause the veins to become enlarged and twisted, leading to the development of varicose veins. Additionally, hormonal changes during pregnancy can weaken the walls of the veins and make the valves less effective, further increasing the risk of varicose veins. Varicose veins that develop during pregnancy often improve or disappear within a few months after delivery. However, some women may experience persistent varicose veins after pregnancy, and may require medical treatment to manage or prevent the condition. Pregnant women can take steps to reduce their risk of developing varicose veins by staying physically active, wearing compression stockings, and elevating their legs as often as possible.
Occupations that involve prolonged sitting or standing.
Occupations that involve prolonged sitting or standing can increase the risk of varicose veins. When a person remains in one position for long periods of time, it can reduce circulation and increase pressure on the veins in the legs, making them more susceptible to damage and inflammation. People who work in jobs that require prolonged sitting or standing, such as office workers, factory workers, and healthcare workers, are at an increased risk of developing varicose veins. To manage and prevent varicose veins, people in these occupations can take steps to improve circulation, such as taking frequent breaks to walk around, stretching regularly, and wearing compression stockings. Changing positions frequently and elevating the legs when possible can also help to reduce the risk of developing varicose veins.
Exercise regularly.
Regular exercise is one of the most effective ways to manage and prevent varicose veins. Exercise helps to improve circulation and strengthen the muscles in the legs, which can help to reduce the pressure on the veins and prevent them from becoming enlarged and twisted. Additionally, exercise can help to maintain a healthy body weight, which can reduce the risk of developing varicose veins. Low-impact exercises, such as walking, cycling, and swimming, are particularly effective for improving circulation and reducing the risk of varicose veins. People with varicose veins or at risk of developing them should aim to exercise for at least 30 minutes a day, five days a week. Before starting an exercise program, it is important to consult a healthcare professional to ensure that the activities are safe and appropriate for individual health conditions.
Low-impact exercises.
Low-impact exercises are activities that are gentle on the joints and do not put excessive strain on the body. These exercises are ideal for people with varicose veins, as they help to improve circulation without putting undue stress on the veins. Some examples of low-impact exercises that are effective for managing and preventing varicose veins include:
- Walking: This is a simple, low-impact exercise that can be done almost anywhere. Walking helps to improve circulation and strengthen the muscles in the legs.
- Cycling: Cycling is another low-impact exercise that is easy on the joints and can help to improve circulation. Riding a stationary bike is a good option for people who prefer to exercise indoors.
- Swimming: Swimming is a great low-impact exercise that works the whole body and can help to improve circulation. The buoyancy of the water also helps to reduce pressure on the veins in the legs.
- Yoga: Yoga is a gentle form of exercise that can help to improve flexibility and reduce stress. Certain yoga poses, such as the Legs-Up-The-Wall pose, can also help to improve circulation in the legs.
By incorporating these low-impact exercises into a regular exercise routine, people can help to manage and prevent varicose veins. It is important to consult with a healthcare professional before starting an exercise program to ensure that the activities are safe and appropriate for individual health conditions.
Walking.
Walking is a simple and effective low-impact exercise that can help to manage and prevent varicose veins. Walking helps to improve circulation in the legs and strengthen the muscles that support the veins. It also helps to reduce blood pressure, which can alleviate some of the pressure on the veins. Walking is a great exercise option because it is free, easy to do, and can be done almost anywhere. To get the most benefit from walking, it is recommended to aim for at least 30 minutes of moderate-intensity walking per day, most days of the week. People with varicose veins should also wear comfortable, supportive shoes and avoid walking on hard or uneven surfaces, which can put additional stress on the veins. If walking for 30 minutes at once is difficult, people can start by breaking it up into shorter, more frequent walks throughout the day. As with any exercise program, it is important to consult with a healthcare professional before starting a new exercise routine to ensure that it is safe and appropriate for individual health conditions.
Maintain a healthy weight.
Maintaining a healthy weight is an important factor in managing and preventing varicose veins. Excess body weight puts additional pressure on the veins in the legs, which can lead to damage and inflammation. People who are overweight or obese are at a higher risk of developing varicose veins, as well as other circulatory problems. Losing weight can help to reduce the pressure on the veins and improve circulation. A healthy diet and regular exercise are the most effective ways to achieve and maintain a healthy weight. Eating a balanced diet that is rich in fruits, vegetables, lean proteins, and whole grains can help to promote weight loss and improve overall health. Regular exercise, such as walking, swimming, or cycling, can help to burn calories and build muscle, which can further support weight loss efforts. If needed, people can also consider working with a healthcare professional or registered dietitian to develop a personalized plan for achieving and maintaining a healthy weight.
Healthy diet.
Eating a healthy diet is an important factor in managing and preventing varicose veins. A healthy diet can help to support healthy circulation, maintain a healthy weight, and reduce inflammation. Some dietary changes that can be helpful for managing and preventing varicose veins include:
- Eating a variety of fruits and vegetables: Fruits and vegetables are rich in vitamins, minerals, and antioxidants, which can help to support overall health and reduce inflammation.
- Consuming high-fiber foods: High-fiber foods, such as whole grains, legumes, and fruits, can help to promote healthy digestion and prevent constipation, which can put additional pressure on the veins.
- Drinking plenty of water: Staying well-hydrated can help to improve circulation and reduce the risk of blood clots.
- Reducing salt intake: Consuming too much salt can contribute to fluid retention and swelling, which can exacerbate the symptoms of varicose veins.
- Avoiding processed and fried foods: Processed and fried foods can be high in unhealthy fats and sodium, which can contribute to inflammation and poor circulation.
By making these dietary changes, people can help to manage and prevent varicose veins. It is important to work with a healthcare professional or registered dietitian to develop a personalized nutrition plan that takes individual health needs and preferences into account.
Portion control.
Portion control is an important aspect of a healthy diet and can be helpful in managing and preventing varicose veins. Eating too much can contribute to excess body weight, which can put additional pressure on the veins and exacerbate the symptoms of varicose veins. In addition to focusing on the quality of the foods we eat, it’s also important to pay attention to how much we are eating. Some tips for practicing portion control include:
- Using smaller plates: By using smaller plates, we can trick our brains into thinking we are eating a full meal, even if the portions are smaller.
- Measuring out portions: Measuring out portions can help to ensure that we are not consuming more than we need.
- Eating slowly: Eating slowly can help to give our brains time to register that we are full and prevent overeating.
- Planning ahead: Planning meals and snacks ahead of time can help to prevent impulsive snacking and overeating.
By practicing portion control, we can help to maintain a healthy weight and reduce the pressure on the veins, which can improve overall circulation and prevent the development of varicose veins. It’s important to work with a healthcare professional or registered dietitian to determine the appropriate portion sizes and dietary needs based on individual health conditions and goals.
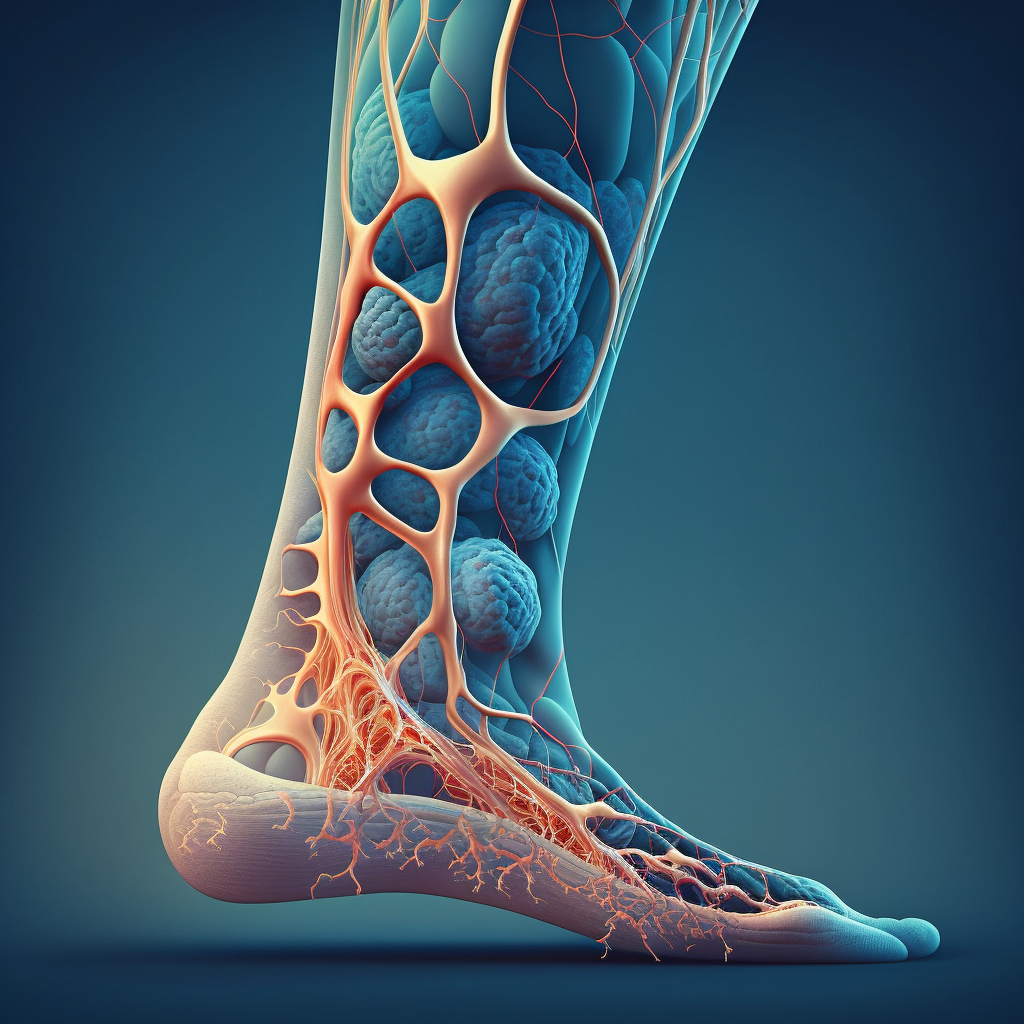
Elevate legs.
Elevating the legs is a simple and effective way to manage the symptoms of varicose veins. Elevating the legs helps to improve circulation and reduce swelling in the legs. To elevate the legs, people can lie down on their back and prop their legs up on pillows or a chair. The legs should be elevated above the level of the heart, which allows gravity to help the blood flow back towards the heart. People can also elevate their legs throughout the day by using a footstool or by taking frequent breaks to lie down and elevate their legs. Elevating the legs for 15-20 minutes, 3-4 times a day, can help to alleviate the symptoms of varicose veins, such as pain, swelling, and fatigue. It’s important to note that elevating the legs is a temporary solution and should be used in conjunction with other management strategies, such as regular exercise and wearing compression stockings, to prevent the progression of varicose veins.
During breaks.
Taking breaks to elevate the legs throughout the day is a great way to manage the symptoms of varicose veins. During breaks, people can take a few minutes to lie down on their back and prop their legs up on pillows or a chair. If lying down is not an option, people can also elevate their legs by using a footstool or by propping their feet up on a stack of books or other objects. It’s important to elevate the legs above the level of the heart, which helps to improve circulation and reduce swelling in the legs. Taking breaks to elevate the legs can also help to reduce fatigue and prevent the development of blood clots. It’s recommended to take breaks to elevate the legs for 15-20 minutes, 3-4 times a day, to effectively manage the symptoms of varicose veins. It’s important to note that taking breaks to elevate the legs is a temporary solution and should be used in conjunction with other management strategies, such as regular exercise and wearing compression stockings, to prevent the progression of varicose veins.
At night.
Elevating the legs at night is a good way to manage the symptoms of varicose veins while sleeping. To do this, people can use a few pillows to elevate their legs while lying down. The pillows should be placed under the calves and feet to lift the legs above the level of the heart. This position helps to improve circulation and reduce swelling in the legs, which can alleviate the discomfort associated with varicose veins. Elevating the legs at night can also help to prevent blood from pooling in the lower legs and feet, which can reduce the risk of developing blood clots. If elevating the legs with pillows is uncomfortable, people can also try sleeping in a recliner or adjustable bed that allows them to elevate their legs. It’s important to note that elevating the legs at night is a temporary solution and should be used in conjunction with other management strategies, such as regular exercise and wearing compression stockings, to prevent the progression of varicose veins.
Wear compression stockings.
Wearing compression stockings is a non-invasive and effective way to manage and prevent varicose veins. Compression stockings are specially designed to apply pressure to the legs and promote blood flow, which can help to alleviate the symptoms of varicose veins, such as pain, swelling, and fatigue. Compression stockings come in different compression levels and styles, ranging from knee-high to thigh-high and pantyhose. It’s important to choose the right compression level based on individual needs and to consult with a healthcare professional or a certified fitter to ensure a proper fit. The compression stockings should fit snugly but not be too tight, which can impede circulation. Compression stockings should be worn throughout the day and removed at night. It’s important to replace compression stockings every 3-6 months or as recommended by the manufacturer or healthcare professional. Wearing compression stockings in conjunction with other management strategies, such as regular exercise and elevating the legs, can help to prevent the progression of varicose veins and improve overall circulation.
Types of compression stockings.
There are several types of compression stockings available, including:
- Gradient compression stockings: These stockings are designed to provide the most pressure at the ankle and gradually decrease in pressure as they go up the leg. Gradient compression stockings are the most common type of compression stockings and are available in different compression levels.
- Anti-embolism stockings: These stockings are designed to prevent blood clots in the legs and are often used during and after surgery or for people who are bedridden. Anti-embolism stockings provide a uniform pressure to the leg to help prevent blood clots from forming.
- Thigh-high compression stockings: These stockings provide compression to the entire leg, including the thigh. They are often recommended for people with varicose veins, edema, or deep vein thrombosis.
- Knee-high compression stockings: These stockings provide compression to the calf and are often recommended for people who stand or sit for long periods of time.
- Pantyhose compression stockings: These stockings provide compression to the entire leg and are often recommended for women who want the benefits of compression stockings while wearing dresses or skirts.
It’s important to choose the right type of compression stockings based on individual needs and to consult with a healthcare professional or a certified fitter to ensure a proper fit. Compression stockings should be worn throughout the day and removed at night.
Proper fit.
Proper fit is essential when it comes to compression stockings. A poorly fitting stocking can cause discomfort, impede circulation, and even worsen the symptoms of varicose veins. It’s important to consult with a healthcare professional or a certified fitter to ensure a proper fit. A professional fitter can take accurate measurements of the legs to determine the right size and compression level of the stockings. They can also provide guidance on how to put on and take off the stockings, as well as how to care for them. It’s important to wear the right size of compression stockings, which should fit snugly but not be too tight. The stockings should be comfortable and provide the right amount of compression to promote blood flow. If the stockings are too tight, they can cause pain, skin irritation, or even lead to blood clots. It’s important to replace compression stockings every 3-6 months or as recommended by the manufacturer or healthcare professional. By wearing properly fitting compression stockings, people with varicose veins can manage their symptoms and improve circulation.
Avoid prolonged sitting or standing.
Avoiding prolonged sitting or standing is an important part of managing and preventing varicose veins. When a person sits or stands for long periods of time, blood can pool in the legs, increasing the pressure on the veins and causing them to stretch and swell. This can lead to the development of varicose veins or make existing ones worse. To prevent this, it’s important to take frequent breaks and change positions throughout the day. If a person has a job that requires prolonged sitting or standing, they can take regular breaks to walk around or stretch their legs. They can also try to shift their weight from one foot to the other or move their legs and feet while sitting. When sitting, it’s important to keep the legs uncrossed and the feet elevated slightly. When standing, it’s important to avoid locking the knees and to shift weight from one leg to the other. By avoiding prolonged sitting or standing and taking frequent breaks, people can improve circulation and reduce the risk of developing or worsening varicose veins.
Take breaks.
Taking breaks is an important part of managing and preventing varicose veins. Prolonged sitting or standing can cause blood to pool in the legs, leading to increased pressure on the veins and potentially worsening existing varicose veins. To prevent this, it’s important to take frequent breaks throughout the day to move around and change positions. This can help improve circulation and reduce the risk of developing or worsening varicose veins. For those who have jobs that require prolonged sitting or standing, taking a break every 30 minutes to an hour is recommended. During these breaks, it’s a good idea to stretch the legs, walk around, or perform light exercises. If possible, elevating the legs during breaks can also help improve circulation. By taking breaks, people can reduce the risk of developing or worsening varicose veins and improve overall leg health.
Flex calf muscles.
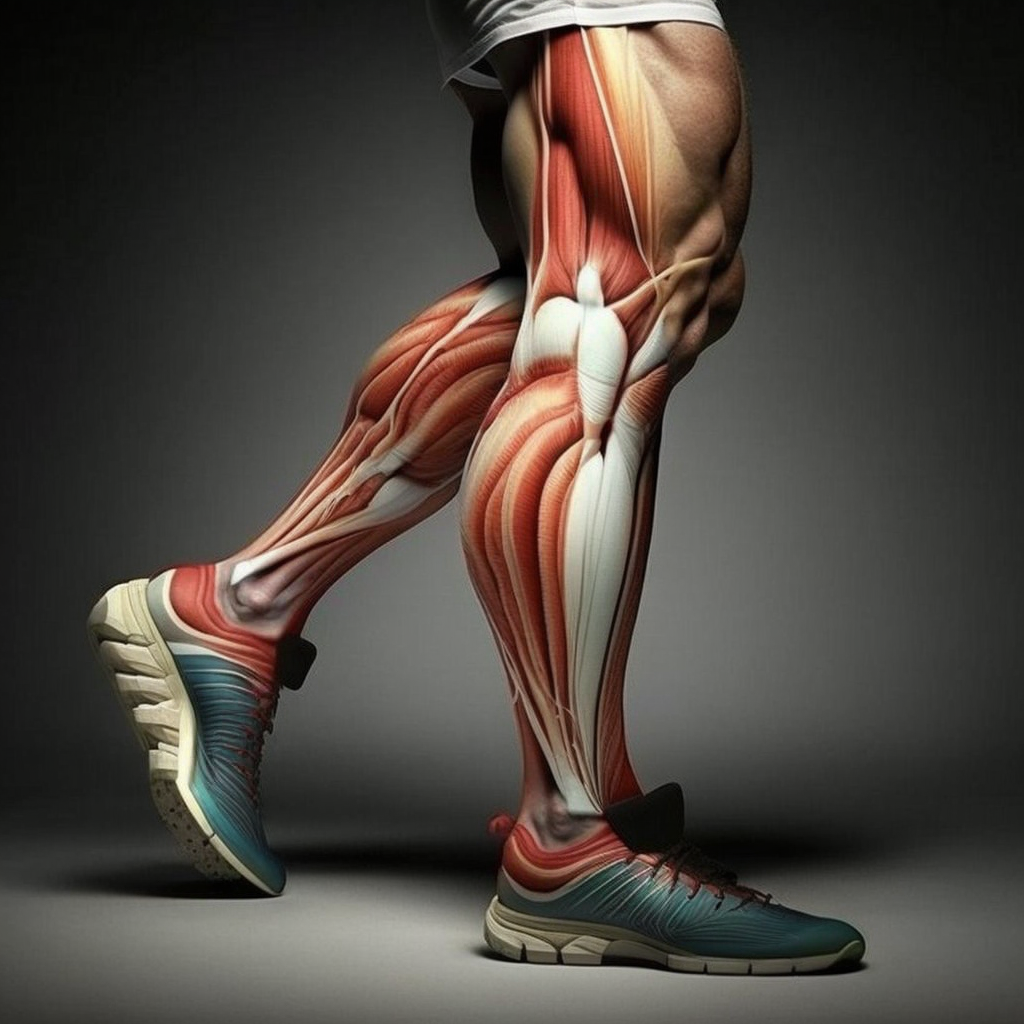
Flexing the calf muscles can help improve circulation and prevent varicose veins. The calf muscles act as a pump to help push blood back up to the heart and improve blood flow. To flex the calf muscles, a person can stand with their feet flat on the ground and slowly raise up onto their toes. Hold the position for a few seconds, then slowly lower the heels back down to the ground. This exercise can be repeated several times throughout the day, especially during prolonged periods of sitting or standing. By flexing the calf muscles, people can help improve circulation and prevent blood from pooling in the legs, which can help reduce the risk of developing or worsening varicose veins.
Endovenous laser treatment.
Endovenous laser treatment (EVLT) is a minimally invasive medical procedure used to treat varicose veins. During the procedure, a laser fiber is inserted into the affected vein, which delivers energy that causes the vein to collapse and seal shut. Blood is then rerouted to healthier veins, and the treated vein is eventually absorbed by the body. EVLT is performed on an outpatient basis, under local anesthesia, and typically takes less than an hour to complete. The procedure is associated with minimal pain, scarring, and downtime. After the procedure, patients are usually advised to wear compression stockings and avoid strenuous activities for several days. EVLT is considered an effective treatment option for varicose veins, with a high success rate and low risk of complications. However, it may not be suitable for all patients, and a healthcare professional should be consulted to determine the most appropriate treatment option based on individual circumstances.
Radiofrequency ablation.
Radiofrequency ablation (RFA) is a minimally invasive medical procedure used to treat varicose veins. During the procedure, a catheter is inserted into the affected vein, which delivers radiofrequency energy that causes the vein to heat up and seal shut. Blood is then rerouted to healthier veins, and the treated vein is eventually absorbed by the body. RFA is performed on an outpatient basis, under local anesthesia, and typically takes less than an hour to complete. The procedure is associated with minimal pain, scarring, and downtime. After the procedure, patients are usually advised to wear compression stockings and avoid strenuous activities for several days. RFA is considered an effective treatment option for varicose veins, with a high success rate and low risk of complications. However, it may not be suitable for all patients, and a healthcare professional should be consulted to determine the most appropriate treatment option based on individual circumstances.
Sclerotherapy.
Sclerotherapy is a minimally invasive medical procedure used to treat varicose veins and spider veins. During the procedure, a healthcare professional injects a solution directly into the affected vein, which causes the vein to collapse and eventually be absorbed by the body. The solution used in sclerotherapy irritates the lining of the vein, causing it to swell and stick together. Blood is then rerouted to healthier veins, and the treated vein is eventually absorbed by the body. Sclerotherapy is typically performed on an outpatient basis, and the procedure takes about 30 minutes to complete. After the procedure, patients are usually advised to wear compression stockings and avoid strenuous activities for several days. Sclerotherapy is considered a safe and effective treatment option for varicose veins and spider veins, with a high success rate and low risk of complications. However, it may not be suitable for all patients, and a healthcare professional should be consulted to determine the most appropriate treatment option based on individual circumstances.
Surgery.
Surgery is a treatment option for varicose veins that is typically reserved for severe cases that have not responded to other forms of treatment. During surgery, the affected vein is surgically removed or tied off, which redirects blood flow to healthier veins. There are several types of surgical procedures that may be used to treat varicose veins, including ligation and stripping, ambulatory phlebectomy, and endoscopic vein surgery. These procedures are typically performed on an outpatient basis, under general anesthesia, and may require a period of recovery and rehabilitation. Surgery is generally considered a safe and effective treatment option for varicose veins, with a high success rate and low risk of complications. However, it is a more invasive form of treatment than other options, and a healthcare professional should be consulted to determine the most appropriate treatment option based on individual circumstances.
Recap of tips for managing and preventing varicose veins.
Sure, here is a recap of the tips for managing and preventing varicose veins:
- Exercise regularly, especially low-impact exercises like walking, to improve circulation and strengthen leg muscles.
- Maintain a healthy weight to reduce pressure on your veins.
- Eat a healthy, balanced diet and practice portion control to manage your weight and promote healthy circulation.
- Avoid prolonged sitting or standing and take frequent breaks to move around and flex your calf muscles.
- Elevate your legs during breaks and at night to improve blood flow and reduce swelling.
- Wear compression stockings that fit properly to support your veins and improve circulation.
- Consider medical treatments, such as endovenous laser treatment, radiofrequency ablation, or sclerotherapy, if your varicose veins are causing significant discomfort or medical problems.
By following these tips, you can help manage and prevent varicose veins and promote healthy circulation in your legs.
Importance of seeking medical treatment if symptoms persist.
It is important to seek medical treatment if your varicose vein symptoms persist, as they can lead to more serious health problems if left untreated. Varicose veins can cause discomfort, pain, swelling, and skin ulcers, and can increase the risk of blood clots and deep vein thrombosis. In addition, varicose veins can be a sign of underlying venous insufficiency, which can lead to chronic venous insufficiency and other complications.
If you have symptoms of varicose veins that are causing you discomfort or affecting your quality of life, or if you are at risk for complications due to your varicose veins, you should consult a healthcare professional for an evaluation and treatment options. Your healthcare professional can help determine the underlying cause of your varicose veins and recommend the most appropriate course of treatment based on your individual circumstances. Early diagnosis and treatment can help prevent more serious health problems and improve your quality of life.